ECG electrodes are vital medical consumables that serve as the bridge between the human body and diagnostic equipment, enabling accurate monitoring of heart activity. These small yet sophisticated devices are essential in both clinical settings and physical therapy scenarios, where precise heart signal tracking can make a significant difference in patient care. As a key component in cardiovascular diagnostics, understanding the construction, types, and proper usage of ECG electrodes is crucial for healthcare professionals and manufacturers alike.
INTCO Medical, a leader in producing high-quality medical devices, recognises the importance of reliable ECG electrodes in delivering accurate health insights. Whether used in hospitals, clinics, or home monitoring setups, these electrodes must meet strict standards to ensure consistent performance. From their multi-layered design to the materials used in their construction, every aspect of an ECG electrode contributes to its ability to capture clear, actionable data, making them indispensable in modern healthcare.
Electrode Types and Features
Construction
ECG electrodes have multiple layers to facilitate the accurate reading of heart signals. Each one has a connector, label, sensing part, backing, gel, and cover. The sensing part often uses silver/silver chloride (Ag/AgCl). This helps steadily change signals. The backing can be made of foam, fabric, or a film that allows air to pass through. The gel can be wet or dry. This changes how well the signal works and how the skin feels.
The material you pick changes how well it works. For example, EKG electrodes do not rust and use energy well. The table below shows how different materials compare:
|
Electrode Material |
Corrosion Resistance |
Water Drainage Efficiency |
Allowable Current |
Contact Resistance |
Energy Efficiency |
Durability |
|---|---|---|---|---|---|---|
|
EKG |
Excellent |
~2.3x copper |
Low |
High |
Good |
|
|
Copper |
Baseline |
Baseline |
Baseline |
Low |
Baseline |
N/A |
|
Graphite |
Stable |
N/A |
N/A |
High |
Lower |
N/A |
|
Conductive Grid |
Good |
Largest after use |
N/A |
Higher |
More consumption |
Better |
Categories
Companies sort ECG electrodes by what they are made of, gel type, connector, and who uses them. Here are some common types:
-
Foam-backed electrodes: These are soft and let air in. They are good for long checks.
-
Non-woven fabric electrodes: These do not let water in and are strong. They are used for normal tests.
-
Breathable film electrodes: These are thin and soft. They work well for kids or people with soft skin.
-
Wet gel electrodes: These send signals fast. They work best on hairy or oily skin.
-
Dry gel electrodes: These do not leave anything behind and are easy to take off.
-
Carbon or metal connectors: Carbon ones let X-rays go through. This helps with pictures.
Some special types are made for babies or can be moved and used again.
Selection Tips
Picking the right ECG electrode depends on what the patient needs. It also depends on what the doctor wants to find out. Here are some things to think about:
-
Some lead systems, like Mason-Likar, lower muscle noise but can change the wave shape.
-
Some systems, like Frank’s, use fewer leads and show vectors but are less exact.
-
EASI systems use fewer electrodes and are less likely to be put in the wrong place.
Even moving an electrode by 1-2 cm can change the ECG. This can cause wrong results in up to 24% of people.
|
Selection Criteria |
Details |
|---|---|
|
Sensitivity to misplacement |
V2 is the easiest to mess up. V3, V4, and V1 are next. |
|
Diagnostic impact |
Putting electrodes wrong can cause false results in 17-24% of cases. |
|
Placement accuracy tools |
Simulators and devices help put chest leads in the right spot. |
|
Machine learning detection |
AI can find most mistakes except some limb lead swaps. |
Tip: Always pick the electrode that fits the patient’s skin, how long it will be used, and what the test is for. This gives the best results.
Common Placement Errors

Typical Mistakes
Many healthcare workers make the same mistakes with ECG electrode placement. The most common problems are:
-
Putting V1 and V2 too high on the chest, above the fourth rib space.
-
Moving V3 to V6 sideways changes how the heart looks on the test.
-
Mixing up precordial electrodes makes the R wave look wrong.
-
Putting the limb leads too close or too far from the body.
-
Using the Mason-Likar system but not writing it down, which changes the QRS axis.
-
Switching limb electrodes, like swapping the right and left arm or leg leads.
These mistakes often happen when people are in a hurry or do not have enough training. Even moving a lead just 2 cm can change the ECG results.
Impact on Readings
Small changes in where electrodes go can make big changes in ECG results. Studies show that moving V1 and V2 up a little can change the P, R, and T waves. This can make the ECG look like there is a heart attack or other heart problem. For example, putting V1 too high can make the P-wave terminal force three times bigger and turn it upside down. These changes can make doctors think someone has an anteroseptal infarction or Brugada syndrome when they are healthy. Swapping limb leads can flip the ECG or make it look like there was an old heart attack. Machine learning tools can help find these mistakes, but putting electrodes in the right place is still the best way to stop errors.
Compliance Risks
Putting ECG electrodes in the wrong place can cause more than just bad readings. Hospitals and clinics must follow strict rules for where to put electrodes. Inspectors check if staff use the right technique. If workers do not follow the rules, the hospital can fail checks or lose device approval. Mistakes in placement can also cause wrong treatments, which can lead to legal trouble or hurt patients. Training and regular checks help lower these risks and keep patients safe.
Best Practices
Skin Preparation
Getting the skin ready is very important for good ECG results. Healthcare workers should use a simple checklist to help the electrodes work well and get clear signals:
-
Check the skin for any cuts or wounds. Do not put electrodes on hurt skin. This helps stop the pain and keeps the signal safe.
-
If there is hair, shave or trim it close to the skin a day before. This helps the electrode stick better and stops the skin from getting sore.
-
Clean the skin with water and a wet towel. Take off any lotion, oil, makeup, or dead skin. Some people may need alcohol wipes, but let the skin dry before putting on electrodes.
-
Rub the skin gently 5 to 10 times. This helps the signal, but do not rub too hard or make the skin red.
-
Put the electrodes flat on the skin. Make sure there are no folds or wrinkles. Keep the wires away from joints so they do not move too much.
-
Check that the electrode polarity is right before starting the ECG.
Tip: Always use electrodes with fresh, wet gel. Store them the right way so the gel does not dry out.
Adhesion and Impedance
Electrodes must stick well and have low impedance for good ECG signals. If the sticky part is weak, electrodes can fall off. This can make the signal bad or lost. Good sticking keeps the electrodes in place when the patient moves. This helps the ECG stay clear.
Impedance must also be low. For ECG electrodes, it should be 50 kOhms or less. If it is over 199.9 kOhms, the device may show a warning. High impedance can change the ECG signal and make it hard to read. Workers can check impedance with a special meter. They can lower it by getting the skin ready the right way. Using the same brand of electrodes helps keep the signal the same every time.
Note: Do not put electrodes on bones, scars, sore skin, or places with lots of muscle movement. These spots can make impedance go up and make the signal worse.
Training
Training helps healthcare workers get better at putting on ECG electrodes. Studies show that learning programs help people know more and feel more sure about ECGs and where to put electrodes.
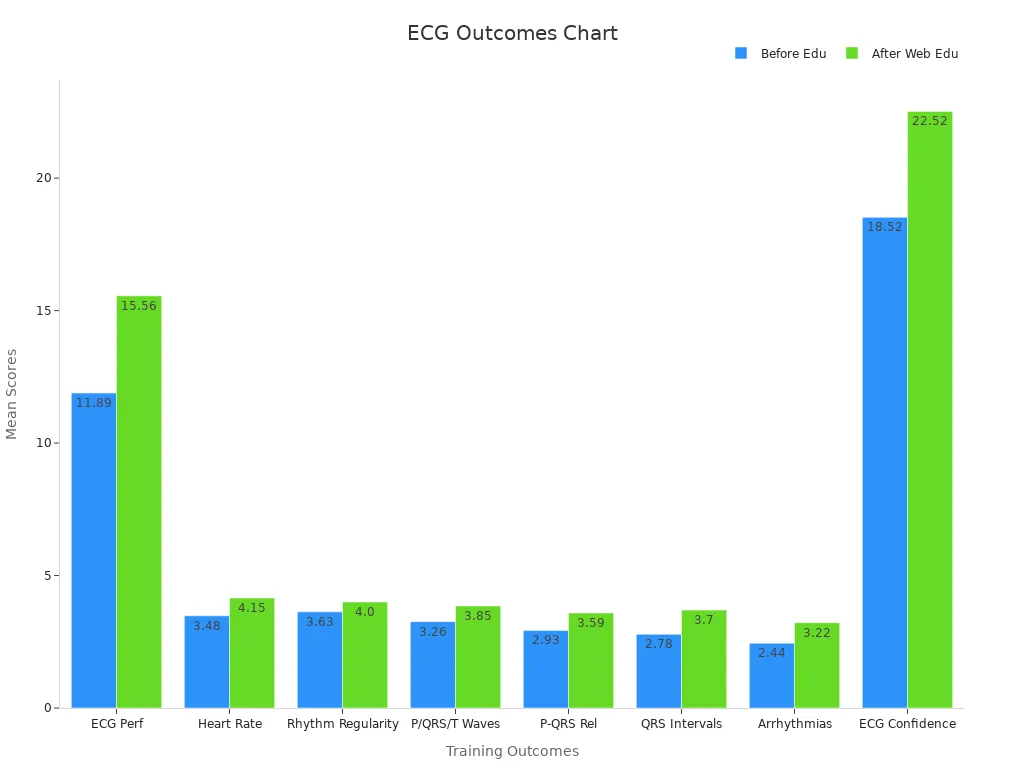
Learning in different ways, like online tools, group classes, and case stories, helps people get much better at ECG skills. Only 37% of nurses learned about ECGs before, but over 96% knew these skills were important. Taking new classes often and using tools like simulators helps keep skills sharp and follow the rules.
Learning all the time and practicing with real tools helps stop mistakes and keeps patients safe during ECG tests.
Healthcare workers in 2025 have to use new rules for ECG electrode placement. Putting electrodes in the right spots helps get the correct results. It also keeps patients safe and follows the rules. Teams that use checklists and learn together do a better job. Learning new things often helps staff know the latest rules.
Knowing the newest information and using the right steps keeps patients safer and helps them get better care.







